“Prevalence and Characterization of Hypoadrenocorticism (HA) in Dogs with Signs of Chronic GI Disease; A Multicenter Study”
– Journal of Veterinary Internal Medicine, June 2020
Key Points:
- 30% of dogs with hypoadrenocorticism are found atypical (exclusive glucocorticoid deficiency therefore electrolytes are normal).
- These cases often present with GI signs (anorexia 89%, vomiting 72%, diarrhea 35%). Other signs included abnormal fecal consistency (mucoid stools, tenesmus, hematochezia, melena).
- GI signs are often chronic (average duration of GI signs of atypical Addisonian is five months). Cause for the GI signs is likely because glucocorticoids are essential for epithelial integrity.
“Atypical Addison’s disease has been found as a cause for chronic GI signs.”
Why This Study Matters: We all tend to think of Addison’s disease as an acute process, but glucocorticoid deficiency (atypical Addison’s disease) often presents with chronic, vague GI signs. Atypical Addison’s disease is much more common than we all expect. Consider hypoadrenocorticism when evaluating chronic or vague GI cases. A baseline cortisol can usually rule out Addison’s disease but if results are flat lined or very low, consider performing a complete ACTH stimulation test.
“Prospective Evaluation of the Influence of Sampling Method on Bacterial Culture Results and Antimicrobial Selection in 52 Dogs with Wounds”
– Journal of Veterinary Emergency and Critical Care, February 14, 2020
Key Points:
- In this study, wound cultures were obtained by three different ways: swab before debridement, swab after debridement and lavage, and swab of actual biopsy.
- Once results were obtained, clinicians were blinded to the techniques used to obtain the culture and asked to choose antimicrobial therapy based on the results.
- The study found that different AMOUNTS of bacteria were obtained depending on sampling technique, but there was no significant difference in which antimicrobials were ultimately chosen by clinicians.
Why this Study Matters: It seems counter-intuitive, but wound cleaning and debridement before culture sampling did not significantly alter bacterial culture results. Bacterial culture can be obtained through various techniques –the way you collect the samples will not affect how you ultimately choose antimicrobial treatment.
Do antimicrobial sutures decrease the risk of surgical site infections? According to a recent study in JAVMA, the answer is NO. Suture site infection was around 6% regardless of whether suture had impregnated antibiotics.
“Randomized, Controlled Clinical Trial to Assess the Effect of Antimicrobial Impregnated Suture on the Incidence of Surgical Site Infections in Dogs and Cats” – Journal of the American Veterinary Association, July 2020
“Welfare of Cats 5-29 Months After Perineal Urethrostomy: 74 cases (2015-2017)”
– Journal of Feline Medicine and Surgery, 2020
Key Points:
- Medical management of blocked cats is standard of care initially, but the reality is that 22-35% of cats will ultimately experience another event.
- Problems however can develop with multiple attempts of medical management (urinary catheterization, cystocentesis etc) which can result in long-standing damage to the urinary system.
- PU cats have some risk of UTIs (one previous study found rates of 22%), but this was not found to be a significant concern in this study.
- PU surgery can result in obstruction, but it was only recognized during the immediate post-operative stage. Long term, these cats did not re-obstruct, and owners in this study reported being very happy with the surgical decision.
Why This Study Matters: Most of the time, PU surgery is recommended after the third obstructive event. The problem with this approach is that repeated medical management (i.e. multiple catheterizations and cystocentesis events) can result in long-standing complications and trauma to the urinary tract system. Consider offering PU surgery after the second blockage, before owners have spent too much on medical management. Owners report feeling excellent QOL following PU surgery.
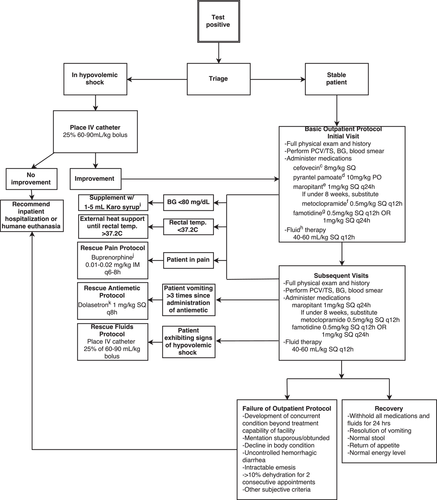
“Retrospective Evaluation of Outpatient Canine Parvovirus Treatment in a Shelter-Based Low-Cost Urban Clinic”
– Journal of Veterinary Emergency and Critical Care, February 2020
Key Points:
- Outpatient protocol offered for parvovirus patients in a shelter setting resulted in an 83% survival rate.
- Hypothermia was found to be a negative prognostic, but low blood glucose values did not appear to affect survival.
- Gaining weight, however, reflected improved survival probability (likely reflects hydration status and food intake).
Why This Study Matters: Let’s face it-treating Parvovirus is expensive and often cost prohibitive for many clients. This article evaluating an option we don’t offer enough to clients who cannot pursue hospitalization: an aggressive outpatient protocol.
This protocol required twice daily outpatient visits for SQ fluids, medications, etc., but on average cost approximately $500 in a shelter setting and had decent outcomes. For committed clients who cannot afford hospitalization but are willing to participate in an involved outpatient care protocol, outcomes are quite successful (Protocol from article below.)