Epilepsy is the most common neurologic condition within the domesticated dog. Epilepsy in itself is a complex disease and by this very nature can make one patient easy to treat while the next drug-resistant. Epilepsy itself is defined as the enduring predisposition of having epileptic seizures.
An epileptic seizure is defined as a transient occurrence of signs and/or symptoms due to abnormal excessive or synchronous neuronal activity in the brain. Common clinical signs of epileptic seizures consist of motor, autonomic and/or behavioral features. Epileptic seizures are classified into two major categories; generalized (tonic-clonic, tonic, clonic, myoclonic, or atonic) or focal epileptic seizures (motor, autonomic, and behavioral). Idiopathic epilepsy is the most common cause of seizures in dogs.
Epileptic seizure activity can be caused from a plethora of etiologies ranging from inherited epilepsy to intracranial disorders, such a developmental/congenital, to extracranial disorders. Extracranial causes are eliminated by performing blood tests to ensure normal hepatic and renal function as well as normal electrolyte homeostasis. When those tests rule out an extracranial cause for epileptic seizure activity, cross-sectional imaging, such as magnet resonance imaging (MRI), of the brain is recommended to rule out gross structural disease processes. Based upon the MRI findings treatment options can be instilled to address the underlying condition. If no abnormalities are found, then a cerebrospinal fluid (CSF) tap and analysis are recommended to rule out inflammatory processes (infectious versus auto-immune) of the brain.
Generally, dogs whose onset of epileptic seizures occurs earlier than six months of age are at greater risk of having been born with structural abnormalities within the brain, (i.e. hydrocephalus) or hepatic disease (i.e. portosystemic shunt). Similarly, dogs whose onset of seizures occurs at an advanced age (older than six years of age) are at greater risk of structural brain disease, particularly brain tumors, although extracranial causes should still be ruled out first (i.e. insulin secreting tumor). Dogs whose epileptic seizures begin between the ages of six months and six years, and in whom no underlying cause can be identified, often are diagnosed as having idiopathic epilepsy.
Types of Epilepsy
Idiopathic epilepsy can be further sub-divided into three categories. Idiopathic epilepsy (genetic epilepsy), when either a causative gene has been identified. Idiopathic epilepsy (suspected genetic epilepsy), when we have confirmed a genetic background (pedigree) linking a genetic predisposition or we have a patient that has a breed documented to have a higher prevalence (>2%) for epilepsy. Lastly, idiopathic epilepsy (epilepsy of unknown cause), when the nature of the underlying cause is yet unknown with no indication of structural brain disease. Regardless of the terminology, therapies are implemented to reduce the frequency and severity of the current epileptic seizure events.
Drug Therapy for Epilepsy
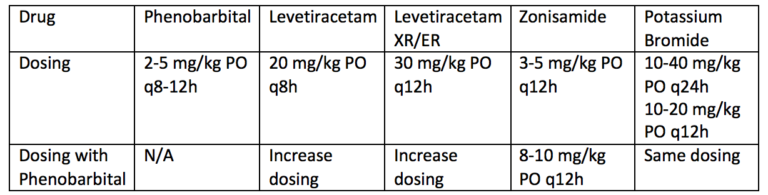
When treating epilepsy, there are many antiepileptic drugs (AED). AED choice depends on many factors such as doctor/client experience, potential side effects, cost, ease of dosing, and how rapid an onset is needed. The most commonly used AEDs are phenobarbital, potassium bromide, zonisamide, and levetiracetam. These drugs may be used alone or in combination to achieve the best control. It is crucial for the client to be involved in selecting a medical therapy for their pet.
- Phenobarbital is still the most regularly and routinely prescribed first-line AED due to its long-standing history and its availability as an injectable formulation.
- Levetiracetam (Keppra) is the second most routinely used AED and this is again due to its availability as an injectable formulation and its significant safety margin. One pitfall of Levetiracetam is that it routinely is prescribed as every eight-hour dosing. The medication does however come in an extended-release formulation that offers the ability to be prescribed every 12-hours. The extended-release formulation does have a draw back as it can only be prescribed for medium and large breed dogs as it only comes in 500mg and 750mg enterically coated tablets.
- Zonisamide is also commonly used but only comes in oral formulations making it less user friendly in the more emergent epileptic. Zonisamide is good a monotherapy, well tolerated, and less frequently reported side effects.
- Potassium bromide rounds out the top four AEDs but is becoming less frequently used. Doses are provided, but it should be remembered that each AED will be started on the low end and titrated up. Based upon clinical improvement of seizures, the maximum dose tolerated, or toxicity will dictate the ceiling of each AED.
Other less frequently used AEDs include topiramate, the benzodiazepine family, gabapentin, phenytoin, valproic acid, and felbamate. Due to cost, the possibility of resistance (tolerance after long-term use), side effects, or increased frequency of administration, these drugs are not our primary choice for the treatment of epileptic seizures in dogs. In some circumstances they can be used as adjunct therapy in combination with other AEDs.
After initiating any AED orally, there is an expected lag time between starting medication and when you will see the maximal effect. Some medications are immediate (i.e. levetiracetam), some take a couple weeks (i.e. phenobarbital and zonisamide), whereas others may take a few months (i.e. potassium bromide). As time goes on, the body starts to metabolize the AED more efficiently and less becomes available within the body to act effectively. Every patient goes through this process to some degree. For this reason, we recommend testing blood levels (i.e. phenobarbital and zonisamide) periodically to ensure the patient is within the therapeutic range (15-45 mcg/mL). Those patients whose levels are too high, often referred to as “toxic range” (>35 mcg/mL), or too low, referred to as “below therapeutic index”, would need their medication regimen (timing, dosing, or addition of adjunct therapy) adjusted. Routine blood work (CBC, Chemistry panel, Urinalysis) and AED level should be performed every two to three months. When performing serum drug levels, it has been reported that there is no statistical difference on whether a “peak” or “trough” sample is taken. If you want to obtain a peak drug concentration, then the sample must be pulled two to four hours after the medication has been administered. If a trough level is to be obtained, then the sample must be pulled just prior to administration of the medication.
What to Expect from Drug Therapy
Management of epileptic seizures often requires long-term care and clients should be forewarned that it can be a difficult and lengthy process. Statistically only about 15% of dogs will become 100% seizure free. Approximately 25% of epileptic patients will be considered refractory or drug-resistant epileptics, meaning they will not respond to traditional therapies. Patients with untreated epilepsy do have a tenancy to get worse over time.
Regardless of the cause of seizures, some generalizations can be made.
- Each seizure episode tends to predispose to more episodes, as the abnormal brain cells encourage other brain cells to behave abnormally.
- Prolonged seizures can be life threatening.
- Intracranial causes of seizure can rarely be cured, so the aim in treatment is to decrease the severity and frequency of the seizures.
- Patients with untreated epileptic seizures do have a tenancy to get worse over time. It is because of this it is imperative that epileptic patients be referred to veterinary neurologist for evaluation, workup, and discussion of therapeutic option before the patient is diagnosed with multidrug-resistant epilepsy.
Alternative Therapies for Canine Epilepsy
Currently, within the realm of veterinary medicine there remains a lack of reported data regarding dietary supplementation for epilepsy management. The novel use of ketogenic diets has been shown to be efficient in reducing seizure frequency and severity in human and dog patients. Ketogenic diets are specialty diets that have been formulated with medium-chain-triglycerides. The most notable constituents being octanoic (C8) and decanoic (C10) triglycerides. The most common supplement being coconut or coconut-derived oil. The true mechanism of antiepileptic action is not yet fully understood.
In the human realm, exploration regarding the use of dietary supplements such as vitamins, minerals, fatty acids, and other nutrients to aid in epileptic seizure control has been made. While some studies have found improvement, other studies have failed to find similar repeatable findings. It is important to keep in mind that with any therapeutic intervention, there is the potential for benefit, the potential to have no effect, or the potential to harm either directly or through a drug-drug or diet-drug interaction. It should be made aware that it is known that different diets and supplements may influence the efficacy, absorption and excretion of AEDs. Because of this fact, it is of utmost importance that veterinary guidance is crucial to provide clients with safe practices with regards to safe drug and dietary combinations and safe feeding practices. With that being said, caution should be exercised when discussing or recommending dietary supplementation products and their administration in the epileptic patient as the complex interplay between medication and diet has not been fully established.
Cannabidiol has recently been making headway for its potential medicinal use. At the present time, there is limited scientific evidence on its efficacy and safety along with its toxicological parameters. In human medicine, it has been documented that the use of CBD oil has increased serum levels of commonly used AEDs. In the dog, we know that cannabis can have toxic effects. For this reason, there are ongoing studies in dogs with epilepsy at Colorado State University that hope to shed light on future use, efficacy and safety of cannabidiol in the veterinary patient.
Whenever there is epileptic seizure activity it is imperative to discuss importance of record keeping with your client. This is to ensure accurate record keeping and to monitor the severity and frequency of the episodes. Based upon this record a determination of seizure frequency can be made and changes to AED therapy can be made promptly. If there are more than three generalized seizures in a 24-hour period, two seizures back-to-back without regaining full consciousness, or there is a seizure that lasts longer than five minutes in duration, it is recommended that the patient be evaluated by either the primary care or emergency veterinarian immediately.
References:
Susan Blades Golubovic and John H. Rossmeisl Jr. J Vet Emerg Crit Care2017; 27(3): 278-287.
Packer R.M.A., Volk H.A., Fowkes R.C. Physiology and Behavior2017; 177: 27-33.
Berk B.A., Packer R.M.A., Volk H.A. Research in Veterinary Science 2018; 119: 276-284.

