What is DKA in Dogs and Cats?
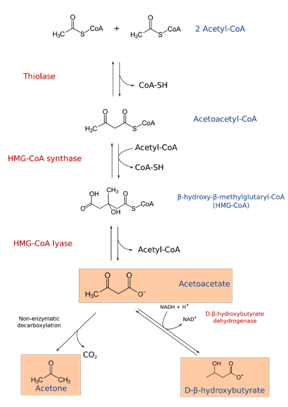
Diabetic Ketoacidosis (DKA) is a serious and life-threatening complication of diabetes mellitus that can occur in dogs and cats. DKA is characterized by hyperglycemia, ketonemia, +/- ketonuria, and metabolic acidosis. Ketone bodies are formed by lipolysis (breakdown of fat) of fat and beta-oxidation when the metabolic demands of the cells are not met by the limited intracellular glucose concentrations. This provides alternative energy sources for cells, which are most important for the brain. The three ketones that are formed include beta-hydroxybutyrate, acetoacetate, and acetone. Beta-hydroxybutyrate (BHB) and acetoacetate are anions of moderately strong acids contributing most to the acidemia (low blood pH). Acetone is the ketone body that can be detected on breath.
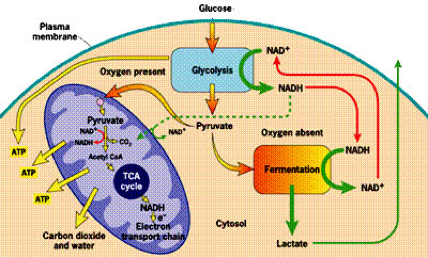
Normal Glycolysis, TCA Cycle, and Electron Transport Chain
In a normal animal, glucose enters the cell (with help of insulin) – undergoes glycolysis to pyruvate within cytosol – pyruvate moves into mitochondria (energy generating organelle in the cell) to enter the TCA cycle and ATP is formed. ATP is the main energy source of the body.
Ketone Formation in Dogs and Cats
When glucose cannot enter the cell, free fatty acids are broken down (lipolysis) and move into the cell to undergo beta-oxidation (creation of pyruvate). The pyruvate then moves into the mitochondria to enter the TCA cycle (by conversion to Acetyl-CoA first). However, when the TCA cycle is overwhelmed, the Acetyl-CoA is used in ketogenesis to form ketone bodies.
Summary of Diabetic Ketoacidosis (DKA) in Dogs and Cats
- When there is no insulin the body cannot utilize glucose and there is no intracellular glucose. The body then uses ketone bodes as an alternate source.
- When there is decreased insulin and increased counterregulatory hormones fatty acids are converted to AcCoA and then ketones. In the non-diabetic, AcCoA and pyruvate can enter the CAC and ETC to form ATP.
- Therefore the increased production of FFA from lipolysis and decreased utilization → KETONES.
Now to the clinically important stuff…
Diagnosis of Diabetic Ketoacidosis (DKA) in Dogs and Cats
There are some differences in the historical and exam findings, risk factors and blood results between dogs and cats. Below are some tips on cats followed by dogs.
Cats
Historical findings: Polyuria, polydipsia, weight loss, anorexia, vomiting and lethargy.
Physical exam findings: Thin body condition, dehydration, icterus and hepatomegaly.
Risk factors: Mean age 9 years (range 2 years to 16 years). No breed or sex predilections. Concurrent disease in 90% of cats with DKA (CKD, acute pancreatitis, hepatic lipidosis, UTI/other infection and neoplasia most common). Most DKA cats are newly diagnosed diabetics.
CBC findings: Anemia, neutrophilia with left shift and Heinz bodies (thought to be correlated to Beta-hydroxybutyrate concentrations).
Biochemical findings: Hyperglycemia, ketonemia, acidemia, elevated ALT, hypercholesterolemia, azotemia, hyponatremia (pseudo), normokalemia or hyperkalemia, normophosphatemia or hyperphosphatemia and hypomagnesemia. Potassium and phosphorus levels will drop with fluid therapy. Azotemia more common in cats than dogs.
Dogs
Historical findings: Polyuria, polydipsia, weight loss, anorexia, vomiting and lethargy.
Physical exam findings: Overweight or underweight, dehydration, cranial abdominal organomegaly, heart murmur, mental dullness, abdominal pain, dyspnea, coughing, abnormal lung sounds and cataracts.
Risk factors: Median age 8 years (range 8 months to 16 years). No breed or sex predilections. Concurrent disease in approximately 70% of dogs with DKA (acute pancreatitis, UTI and hyperadrenocorticism most common). 20% have UTI.
CBC findings: 50% of dogs have non-regenerative anemia. Neutrophilia with left shift and thrombocytosis also common.
Biochemical findings: Hyperglycemia, ketonemia, acidemia, elevated ALP (almost all dogs with DKA). Elevated ALT, AST and hypercholesterolemia in approximately half of dogs. Hyponatremia (pseudo), normokalemia or hyperkalemia, normophosphatemia or hyperphosphatemia and hypomagnesemia. Potassium and phosphorus levels will drop with fluid therapy. Hypchloremia and decreased ionized calcium concentrations in approximately 50% of dogs with DKA. Hyperlactatemia in approximately 1/3 of dogs.
BHB is the first ketone body formed but isn’t detected in the ketone sticks. Ketones develop in the blood before the urine so you can use plasma to diagnose for ketones earlier. This can be done on the urine dipsticks that look for ketones so there is no need for additional equipment.
Treatment of Diabetic Ketoacidosis (DKA) in Dogs and Cats
Goal of treatment of DKA in dogs and cats is rehydration, drop glucose, normalizing pH, eliminate ketones, manage electrolyte imbalances and address concurrent diseases or underlying disease.
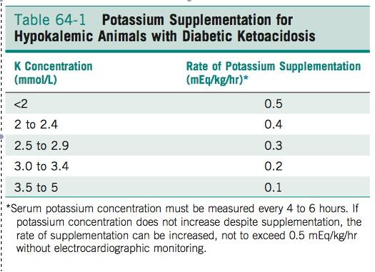
Treatment includes aggressive fluid therapy (most important), potassium and phosphorus supplementation, insulin therapy and possible bicarbonate administration (rarely needed).
Fluid Administration Tips
- Administration of 0.9% NaCl fluid can be used because of high sodium content. However, this may contribute to acidosis so Lactated Ringers Solution (LRS) and Plasmalyte (P-lyte) are fine as well and may help to alkalinize.
- Fluids are given for approximately 6 hours before any insulin therapy is attempted because fluids alone will drop glucose concentrations.
- Potassium chloride (KCl) can be given as a CRI at no more than 0.5 mEq/kg/hr.
- KPhos can be given as a CRI at 0.03-0.12 mM/kg/hr. Alternatively, can use the other potassium supplementation scale (how much mEq to add to 1 L) by using half KCl and half KPhos.
Insulin Therapy
Insulin therapy is also a mainstay of DKA therapy. Two main protocols include regular insulin constant rate infusion (CRI) or regular insulin intermittent intramuscular (IM). The blood glucose (BG) is measured every 2 hours with CRI. BG is measured every hour with IM.
- IM: initial dose of 0.2 U/kg regular insulin, followed by 0.1 U/kg 1 hour later. Then base insulin dose on how much glucose is dropping per hour. If drops more than 75 mg/dl/hr, use 0.05 U/kg/hr. If drops 50-75 mg/dl/hr, use 0.1 U/kg/hr. If drops less than 50 mg/dl/hr, use 0.2 U/kg/hr.
- CRI: ***Note*** Must run 50 ml through the IV set before setting up to patient because insulin binds to plastic! Different clinicians will likely have slightly different CRI protocols.
Bicarbonate Therapy
Bicarbonate therapy is described but is only reserved for severely acidemic patients (generally, pH less than 7 after 1 hour of fluid therapy per American Diabetes Association). This is not commonly performed. Risks in humans include cerebral edema, increased ketogenesis, worsening hypokalemia, and paradoxical cerebral acidosis. One protocol is: administer 1/2 to 1/3 of a (0.3 x body weight (kg) x negative base excess) dose over twenty-minute interval every hour.
More Tips & Notes on DKA
- In humans, a rise in glucose of 62 mg/dl accounts for a decrease in 1 mEq/L of sodium. In dogs a rise of 100 mg/dl decreases Na by 1.6 mEq/L
- Urine dipstick test reacts with acetoacetate and not Beta-hydroxybutyrate. Serum Beta-hydroxybutyrate measurement is better than measuring for urine ketones (can be ketonemic without being ketonuric).
- Approximately 20% of dogs have positive aerobic growth on urine culture.
- Differentials for ketonemia include acute pancreatitis, starvation, low-carb diet, persistent hypoglycemia, persistent fever, and pregnancy.
- Differentials for primary metabolic acidosis include acute kidney injury, lactic acidosis, toxins, severe tissue destruction, renal tubular acidosis, and hyperchloremia.
- Almost all dogs and only young cats get cataracts associated with diabetes mellitus because glucose enters the lens of the eye and is metabolized by the polyol pathway to sorbitol and fructose, which then promote water to enter the lens causing disruption of lens fibers. The enzyme responsible is called aldose reductase (dogs have high activity of aldose reductase their entire lives where cats tend to lose activity of this enzyme as they age).
- Hormones that further antagonize insulin include cortisol, glucagon, epinephrine, growth hormone, and progesterone.
- Glucagon most implicated…with severe cellular starvation for glucose, glycogenolysis and gluconeogenesis are ramped up which worsens hyperglycemia.
- Vomiting often occurs due to activation of chemoreceptor trigger zone by ketones.
- Degree of acidosis in dogs is associated with poor outcome.
- Most patients with DKA survive to discharge. Approximately 70% of dogs and cats survive to discharge. Median hospitalization is 6 days (dogs) and 5 days (cats). Approximately 7% of dogs and up to 40% of cats experience DKA again. Dogs with concurrent Cushing’s are less likely to leave the hospital.
- Hyperglycemic Hyperosmolar Syndrome (HHS) is an uncommon form of a diabetic crisis that can occur in dogs and cats. Learn more with this article.

